Common Skin Conditions
PSORIASIS
The National Psoriasis Foundation describes psoriasis as an immune disease affecting approximately three percent of the American population.
Immune diseases stem from faulty signals in the body that typically have no known cause and result in widespread inflammation. The most obvious signs of psoriasis are scales on the skin and raised plaques. The appearance of plaques can be considerably different based on skin tone and type of psoriasis.
Understanding the Immune System’s Faulty Messaging to the Skin
When you have psoriasis, your immune system instructs your skin cells to grow faster than they should. New skin cells normally replace old skin cells monthly. However, the faulty response of psoriasis means your body does not have the chance to keep up with the growth. Rather than shedding old skin cells as your body would normally do, skin cells pile on top of each other and cause dry, red, and flaky patches to appear.
Psoriasis causes new skin cells to grow in only three to four days instead of the typical 30 days. The most common symptoms associated with psoriasis include itching, stinging, and burning sensations. You can develop scales or plaques anywhere on your body, but they are most likely to appear on the scalp, elbows, knees and lower back. Most people develop psoriasis between the ages of 15 and 25, and it is generally a life-long condition. It affects men and women equally. Children can also develop this immune condition.
The overall health of your immune system and the genetic traits you receive from each parent both play a role in whether you will develop psoriasis. Infection, stress and injuries can trigger psoriasis, but the exact cause of the flare-ups remains unknown.
The Five Different Types of Psoriasis
You could have one of five types of psoriasis or a combination of any of the types described below.
Erythrodermic:
This type is exceptionally rare, affecting just two percent of psoriasis sufferers. The primary symptoms of erythrodermic psoriasis are intense reddening of skin and skin that sheds in large sheets rather than small patches.
Guttate:
Approximately eight percent of people with psoriasis have this type. Common symptoms include small, round red spots on the torso, arms, legs, or anywhere else on the body.
Inverse:
Up to 25 percent of people with psoriasis have this type. The most common symptoms are deep red spots and itchiness in the skin folds, including underneath the breasts, genital areas, buttocks, and underarms.
Plaque:
Plaque psoriasis is the most common type of psoriasis, affecting approximately 80 percent of people with this immune response condition. Plaques are often itchy and painful, and depending on your skin tone, they can appear purple, red, or silver. This type impacts 80-90% of psoriasis patients.
Pustular:
Roughly three percent of people with psoriasis have this type. You will notice white painful pus-filled bumps that may or may not have reddened skin surrounding them. These bumps can be on one or two areas of the body or may cover the entire body. The pus in these pustules is caused by inflammation and is not contagious.
Psoriasis is treatable, and Anne Arundel Dermatology is here to help. To learn more about treatment options which include topical and systemic medications as well as phototherapy, contact us to schedule an appointment with one of our providers. For more information about two safe and effective treatment options, visit our pages on Excimer Laser Therapy and Phototherapy.
ECZEMA
Eczema is a common skin condition that also goes by the names atopic eczema, dermatitis, and atopic dermatitis. The condition, which is especially common in children, causes red patches to appear on the skin that are scaly, itchy, and dry.
Who Gets Eczema, and How Long Does It Last?
This skin condition frequently appears in children during their first year of life. The itching caused by eczema can be so intense that some babies and toddlers may not be able to sleep. Since they do not fully understand how to scratch itchy skin to make it feel better, very young children may rub their skin against the nearest surface in an attempt to find relief. Eczema is not contagious.
Skin rashes can make children feel uncomfortable and may require treatment to avoid secondary infection. Parents can also take steps at home to reduce the likelihood of an eczema flare in their child. For example, babies and toddlers with eczema are often sensitive to the dyes used in soaps and laundry detergents. Parents should choose products without these added ingredients. They also need to moisturize their child’s skin regularly.
Some people who develop eczema during childhood continue to deal with the uncomfortable symptoms into their adulthood. They may go several years between flare-ups. Although it is less common, some people never develop eczema during childhood and do not notice their first symptoms until they are adults.
What Causes Eczema?
One of the essential roles of healthy skin is to retain moisture that protects the body from allergens, bacteria, and irritants. People with eczema appear to have variations in their genes that prevent the skin from performing this function effectively. Children who already have food allergies are more prone to developing eczema. Other risk factors include having a family history of eczema, seasonal allergies, asthma, or hay fever.
Common Symptoms of Eczema
Keep in mind that the symptoms of eczema can vary significantly between children and adults and from one person to the next. Here are some typical indications that you or your child might have eczema:
- Cracked, dry, thickened, or scaly skin
- Patches of skin that are brownish-gray or red in color that appear on the upper chest, hands, wrists, neck, feet, ankles, eyelids, and inside the bend of the knees and elbows. Children may also have eczema patches on their cheeks or scalp.
- Raised bumps that can crust over when scratched and leak clear fluid.
- Severe itching.
- Skin that appears swollen, thickened or raw due to intense and chronic scratching.
You or your child may have developed a secondary skin infection if you notice oozing pus, yellow scabs, or red streaks on the skin. Please seek treatment from Anne Arundel Dermatology immediately in this situation to prevent the infection from spreading or getting worse. We recommend a combination of home remedies and professional dermatology treatment for eczema to ensure healthy skin for a lifetime. Left untreated, eczema can cause significant problems with sleep and quality of life.
Please contact our dermatology providers today to learn more about safe and non-invasive treatment options for eczema.
MOLE & SKIN TAGS
People typically have between 10 and 40 moles on their skin but may have more if their skin has a light complexion. The medical name for a mole is a “melanocytic nevus,” and they are typically less than half an inch in diameter.
Moles come in a variety of colors, including black, brown, tan, red, a combination of red and brown, or skin-colored. The moles on your body may be perfectly flat or raised.
Most moles appear on the skin during childhood and adolescence. Moles will grow as the child (or teen) grows. Some moles will darken, and others will lighten. These changes are expected and seldom a sign of melanoma, the most-serious skin cancer.
Moles Represent a Small Imperfection of the Skin
There is a normal distribution of pigment cells (melanocytes) throughout the epidermis (top layer of skin), and there is a ratio of approximately 1 melanocyte for every 36 keratinocytes (skin cells). Your body develops moles when these normally solitary melanocytes grow together to form a nest of cells. Melanocytes are responsible for producing the pigmentation of your skin. They can appear anywhere on the body but are most common on the trunk in men and on the legs in women.
However, we caution you not to assume that every flat or raised mark displaying one more color mentioned above is a mole. Several other types of skin lesions can initially look like a mole. These include:
- Basal cell carcinoma
- Café au lait spots
- Dermatofibromas
- Freckles
- Lentigines
- Liver spots
- Melanoma
- Neurofibromas
- Skin tags
- Seborrheic keratoses
No matter how many moles you have or their location on your body, frequent sun exposure can increase their size and number. Since moles can become cancerous, it is important to protect yourself from the ultraviolet rays of the sun when you are outdoors. Wear sunscreen daily, lightweight clothing, sunglasses, and a wide-brimmed hat, and try to avoid direct exposure between 10:00 a.m. and 4:00 p.m. The sun’s ultraviolet rays are most intense during these hours and can cause sunburn or other damage to your skin.
You Can Still Get New Moles as an Adult
Many people have all the moles that will ever develop on their skin by the time they are a year old. However, others continue to develop new moles into their 20’s and 30’s. It is uncommon for new moles to develop after age 35. If you notice the growth of new moles or a significant change in an existing mole, be sure to schedule an appointment with one of Anne Arundel Dermatology’s dermatologists as soon as possible. We will confirm or rule out the possibility of skin cancer and treat your moles accordingly.
Types of Moles and How to Spot Changes
The three types of moles that grow on the human body can be regular and symmetrical, irregular, or cancerous. You will notice one or more of the following when a mole is atypical or cancerous:
- A – Asymmetrical – one half of the mole does not look like the mirror image of the other half.
- B – The borders of the mole are jagged or otherwise irrgular.
- C – Colors have changed.
- D – The diameter is larger than a pencil eraser.
- E – The mole’s appearance has evolved in some way, and has changed from what it has looked like in the past
Dermatologists refer to this method of checking your moles at home as the ABCDE’s of melanoma. Although a cancerous mole sounds scary, the good news is that it is highly treatable in the early stages. Performing regular skin checks at home and requesting an appointment anytime you notice something unusual is the best way to stay ahead of skin cancer. You can learn more about skin cancer at this link or contact our dermatology practice with additional questions.
ACNE
More than 90 percent of American teenagers and young adults deal with acne, with the peak age being 17 to 18 for women and 19 to 20 for men. Acne is generally associated with teenagers, but this skin concern doesn’t necessarily disappear once you reach adulthood.
Acne is an extremely common skin condition that develops when hair follicles on the face become clogged with dead skin cells and oil.
Causes and Triggers of Acne
Besides your face, acne can appear on your upper back, shoulders, chest, and forehead. The reason acne strikes in these areas is that they have the most sebaceous glands, also known as oil glands, than other parts of the body. Hair follicles and oil glands remain permanently connected.
Four main factors cause acne:
- Excess oil production
- Hair follicles getting clogged
- Bacteria
- Inflammation in the follicle
Hormones and medication may contribute to acne
Types of Acne
- Whiteheads
- Blackheads
- papules
- pustules
- Nodules
- cystic lesions
You can have a combination of any of these types of acne:
Blackheads
Named after the color they produce, blackheads contain oil and dead skin cells and are open to the surface. The reaction of oil to air is what causes this type of acne to turn black.

Papules
Papules are small pink or red bumps that have become inflamed. They can feel sensitive to touch.
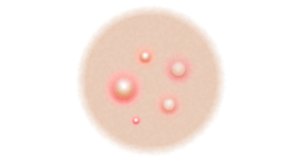
Pustules
This is another type of inflamed pimple. They look like whiteheads except they have a ring around the bump that contains yellow or white pus.
Cystic
Painful, pus-filled lumps under the skin
Nodules
Large, solid, painful lumps under the skin
Whiteheads
This type of acne has a closed surface and is white in appearance. Whiteheads develop when oil and skin cells clog pores and prevent them from opening.
Maskne
Millions of Americans have been wearing masks every day for the past two years to help protect themselves and others from the COVID-19 virus. Unfortunately, frequent mask-wearing can cause skin problems similar to acne. Sweat and friction caused by the mask rubbing against the skin are the primary causes of this type of acne. Be sure to wash your mask often and change disposable masks daily.
Acne is Treatable
Anne Arundel Dermatology offers acne treatments for all ages ranging from laser therapy to topical prescriptions that may show results in as little as a few weeks. You may also want to consider microneedling if you have acne scars. Please contact us to request a consultation.
RASHES
Rashes can be a frustrating and uncomfortable experience. Identifying the type of rash you have is the first step in understanding how to treat it. Our team of dermatologists will evaluate your skin and provide an accurate diagnosis. From there, we’ll create a personalized treatment plan to help you find relief from your rash.
Types of Rashes
Rashes can be caused by a variety of factors, including infections, allergies, and certain medical conditions. There are many types of rashes, each with its own characteristics and causes. Understanding the different types of rashes can help you identify the cause of your rash and seek the appropriate treatment. Types of rashes include:
Infectious Rashes
Bacteria, viruses, or other pathogens cause infectious rashes. This type of rash is highly contagious and may be spread through contact with infected individuals, respiratory droplets, or contaminated surfaces. Common examples of infectious rashes include:
- Chickenpox
- Measles
- Impetigo
- Scarlet Fever
If you suspect you or a loved one has an infectious rash, it is crucial to seek medical attention as soon as possible to prevent the spread of the infection. A physician can diagnose the rash, provide advice on managing symptoms, and deliver any necessary treatments.
Allergic Rashes
Allergic rashes are caused by a reaction to certain substances, such as food, drugs, or environmental allergens, such as poison ivy. These types of rashes can range in severity and are often characterized by red, itchy skin with hives or bumps. Some common allergic rash triggers include pollen, pet dander, insect stings, latex gloves, and certain medications.
Identifying the cause of an allergic rash is important to prevent future reactions. If you are experiencing an allergic rash and are unsure of the cause, we recommend consulting with a dermatologist.
Inflammatory Rashes
Inflammatory rashes are caused by inflammation in the skin. These types of rashes can be triggered by a variety of factors, including infections, allergies, and certain medical conditions. Common examples of inflammatory rashes include:
- Eczema: A chronic condition that causes the skin to become red, itchy, and inflamed. It can affect any part of the body but is most commonly seen on the face, hands, and feet.
- Psoriasis: A long-term skin condition characterized by itchy, red patches of thickened, inflamed skin covered with silvery scales. Psoriasis has the ability to spread throughout any part of the body. However, it is most visible on the scalp, elbows, and knees.
- Dermatitis: A general term that refers to inflammation of the skin. There are several different types of dermatitis, including contact dermatitis (caused by contact with an irritant), atopic dermatitis (a chronic, genetic skin condition), and seborrheic dermatitis (a common form of dermatitis that affects the scalp).
Heat Rashes
A heat rash, also known as prickly heat or miliaria, is a skin irritation caused by blocked sweat glands. It may occur when the body’s natural cooling mechanism becomes impaired, such as during periods of high humidity or when wearing too much clothing in hot weather. Heat rashes are more common in infants and young children, as their sweat glands are not fully developed and may be more prone to becoming blocked.
Autoimmune Rashes
Autoimmune rashes are caused by the immune system attacking the body’s own tissues. These types of rashes can be triggered by various autoimmune conditions, including lupus, scleroderma, and rheumatoid arthritis.
Autoimmune rashes are often characterized by red, scaly, and inflamed skin. They may affect any part of the body but are most commonly seen on the face, scalp, and hands. In some cases, autoimmune rashes may be accompanied by other symptoms, such as joint pain, fatigue, and fever.
Treatment Options
Treatment options for rashes often depend on the cause. For example, infectious rashes may require a course of antibiotics, while allergic rashes may be treated with antihistamines and topical creams. Our team of experienced dermatologists can provide you with a customized treatment plan to address your rash and help you feel better as quickly as possible.
If you are experiencing a rash that does not improve after self-care at home, contact Anne Arundel Dermatology for an evaluation. Common treatment options for rashes include:
- Topical Creams and Ointments
- Oral Medications or Injections
- Phototherapy
- Immunosuppressive Medications
- Antifungal or Antibacterial Medications
ALOPECIA AREATA
The term alopecia areata refers to an autoimmune form of hair loss that is often patchy. Alopecia areata can cause hair loss on the scalp, face, and potentially other areas of the body.
This condition can appear at any age, but it frequently begins in childhood or young adulthood. Hair loss is generally sudden and often begins as round or oval, smooth balding patches. The hair that falls out sometimes grows back, only to fall out again and repeat the cycle. Hair loss occurs when your immune system attacks hair follicles, which are the roots of each strand of hair. Without treatment, hair loss may remain the same or it may worsen. However, with treatment, hair loss may begin to improve in as little as 6 weeks. It is important to know that the hair follicles remain alive in this condition, so improvement and even full regrowth of hair is possible. This condition is not contagious.
Types of Hair loss:
Hair loss may be patchy on the scalp, face or beard (Alopecia barbae). Hair loss may also occur in a band-like distribution on the scalp (Alopecia ophiasis).
Alopecia totalis is the term used when a person has lost all of the hair on their scalp.
Alopecia universalis is the term used when a person has lost all of the hair on their scalp, face and everywhere else on their body.
Symptoms of Alopecia Areata:
- Rows of tiny dents on the fingernails are referred to as pitting or stippling.
- Hairs appear narrow at the base and resemble an exclamation point when regrowth begins.
People with alopecia areata are more sensitive to damage from the sun. We recommend that you protect your ears, face, and head with a wide-brimmed hat whenever you spend more than a few minutes outside.
Although we cannot prevent your hair loss, we can help you re-grow your hair if that is what you desire. Typical treatment options include topical corticosteroids, topical or oral minoxidil, topical anthralin, intralesional corticosteroids, JAK inhibitors and other medications that work on the immune system. Please schedule a consultation with us today to learn more.
WARTS
Warts are round skin growths that appear in response to the human papillomavirus (HPV) infecting your top layer of skin.
They are not cancerous. HPV typically occurs after you have accidentally cut your skin or damaged it in some other way. The virus that causes warts is contagious, which means you can spread it to other parts of your body or to another person.
What Do Warts Look Like?
Most warts are the same color as your skin, but they can also be a darker brown or a combination of gray and black. They are typically flat and feel smooth to the touch. Some warts are painful, and most go away on their own without any treatment. However, some are persistent and can remain for years despite your attempts to treat them at home.
Understanding the Different Types of Warts
You could develop one of five types of warts, each of which has a unique presentation and appears on different parts of the body. These include:
Common Warts:
Typically present on the fingers and toes, common warts have a rounded top, grainy appearance, and can feel rough when touched. They appear grayer in color than the skin surrounding them.
Filiform:
These warts grow around the nose, mouth, neck, and under your chin. They consist of a tiny flap of skin that is the same color as the rest of your skin.
Flat:
Flat warts are not always immediately recognizable because they are quite small and grow on your arms, face, or thighs. They have a flat top and appear as though someone has scraped them, but that usually is not the case.
Periungual:
Periungual warts can be painful because they grow underneath and around fingernails and toenails, impeding their growth.
Plantar:
Plantar warts are unique because they grow into the skin instead of from the skin. You can find them on the bottom of your feet. Plantar warts make the skin around them feel hard and can also make walking uncomfortable.
Can You Treat Warts at Home?
Some wart treatment kits that you buy at a drugstore can be effective in treating warts. You just need to keep a few important things in mind. First, do not try to remove warts that appear on a sensitive part of your body like your mouth, nose, or nostrils.
You also should not treat warts at home if you have diabetes, as diabetes can cause a loss of sensation in the feet and hands. You could injure yourself without realizing it. If you use a wart removal kit that requires you to rub ointment on the wart with a fingernail file or other common instrument, throw the item away after treating the wart. Warts are extremely contagious, and anyone who comes in contact with the file could develop warts themselves.
Anne Arundel Dermatology offers several safe and effective treatment options for stubborn warts. We invite you to schedule an appointment today or contact us with additional questions.
WHITE SPOTS/NAIL FUNGUS
Nail fungus develops from a fungal infection of the fingernails or toenails. A yellow or white spot underneath the tip of the nail is often the first indication of nail fungus.
Left untreated, the fungus can spread deeper into your nail and cause it to crumble, thicken, or become discolored. You may also experience pain.
Anyone can develop nail fungus, although it is rare in children under six. Lifestyle factors, age, and health all determine whether you will develop nail fungus at some point in your life.
Who Develops Nail Fungus?
Your risk of fungus growing in your fingernails or toenails increases with age. People who live in hot and humid clients also develop this condition more often, as do those with the following health conditions:
- Athlete’s foot or another type of fungus-related skin infection
- Cancer treated by chemotherapy
- Diabetes
- Hereditary factors
- Nail infection Recent nail injury or surgery
- Poor circulation in your hands or feet
- Psoriasis
- Previous organ transplant
- Weakened immune system
Certain lifestyle factors also contribute to nail fungus. These include:
- Smoking
- Spending a lot of time in water
- Walking barefoot in a locker room, public shower, pool, or any place that attracts heat and humidity
- Wearing plastic gloves frequently for several hours at a time
- Wearing closed-toe shoes that fit tightly or cause your feet to sweat
- Your hands and feet are regularly wet throughout the day
How Does Nail Fungus Develop?
Microscopic organisms called fungi, which is the plural form of fungus, are responsible for causing an infection in your fingernails or toenails. The most common way that people pick up a fungus is through direct contact with someone else who has a fungal infection. Ringworm and athlete’s foot are two typical examples. Another common way to develop nail fungus is by sharing a fingernail or toenail cutter with someone who already has an infection.
Nail fungus is not always contagious. It can be contracted when a small cut in the skin around your nails presents an opening for the fungus. It can also develop due to a separation between the nail and toe or finger or because of a crack in the nail.
Available Treatments for Nail Fungus
If you think you have fungus growing under a nail, please contact Anne Arundel Dermatology for an appointment. Your dermatologist will trim the affected nail and scrape away the debris underneath it. You will also need to take some type of medication to get rid of the nail fungus.
Mild infections usually respond well to a medicine that you apply directly to the infected nail. The medication prevents new infections from forming while you eliminate the existing fungus. Deep fungal infections require more aggressive treatment with antifungal pills. The FDA has currently approved Fluconazole, Griseofulvin, Itraconazole, and Terbinafine for this purpose.
Combination treatment types and nail removal are additional options. Surgically and non-surgically removed fingernails grow back in about four to six months, while toenails take 12 to 18 months to regrow. Please contact us with additional questions or to request an appointment.
INGROWN TOENAILS
Ingrown toenails are a common foot condition that develops when the corner of a toenail grows into the skin around the nail instead of over it. They occur most often with the big toes.
The issue is usually not serious. However, people with certain medical conditions that affect circulation in the feet are at greater risk of developing ingrown toenails that could potentially cause an infection.
What Causes Ingrown Toenails?
- Poorly fitting shoes especially those with pointed toes such as high heels
- Tearing the corner of your toenail
- Trauma to a toe, such as hitting it against a coffee table or dropping something on it
- Cutting the toenails too short or too rounded – toenails should be cut straight across so that the top of the nail is a straight line.
Most people can manage ingrown toenails on their own at home. You just need to know what to look for to ensure that you do not actually have a different foot problem.
Typical Symptoms of Ingrown Toenails
The first thing you are likely to notice with an ingrown toenail is that the skin around your nail gets inflamed and feels hard and swollen. Bacteria can enter your skin if your toenail grows into the skin or the skin grows over the edge of the nail. You could develop an infection that requires treatment from our dermatology practice. The following are common indications that you have an infected toenail:
- The toe feels warm to the touch and/or appears red
- New onset of pain
- Swelling
- Pus or liquid leaking from your toe
You will need prompt medical attention if you develop an infection or you have an ingrown toenail along with one of these conditions:
- Diabetes
- Poor blood circulation
- Severe nerve damage
Treating Your Ingrown Toenail at Home
Soaking your foot twice a day in warm water and Epsom salt helps to loosen the ingrown toenail and allows it to grow normally. Be sure to keep your feet warm and dry the rest of the time. To relieve pain in your toe, gently lift the edge of the toenail and place dental floss or cotton between your toenail and skin. Next, rub antibiotic cream onto your toenail and cover it with a clean gauze pad. You will need to change the pad each day.
Plan to wear loose-fitting shoes or sandals as your toe heals to prevent your footwear from causing pressure and additional pain. If you still have pain after going through each of these steps, take acetaminophen or ibuprofen to relieve it. Do not attempt to cut the ingrown toenail yourself, since it could make the problem worse.
Feel free to contact Anne Arundel Dermatology if your symptoms do not go away in a few days or if you feel concerned about a possible infection.
Schedule an Appointment
At Southern Dermatology, we are trained to place the well-being and safety of our patients above all else. Our doctors combine a deep understanding of dermatology with advanced medical aesthetics to help minimize the signs of aging. Schedule a visit for any skin condition. Your best skin awaits!

